Advance health care directives are legal documents that allow individuals to express their preferences for medical treatment and care in the event that they become unable to make or communicate their own decisions. A person may become unable to make decisions for themselves due to a medical condition, such as a coma, severe dementia, or a terminal illness. These directives provide guidance to health care providers and loved ones about the individual's medical care preferences, including end-of-life care and life-sustaining treatments. In the United States, advance health care directives are primarily governed by state laws. However, the federal Patient Self-Determination Act (PSDA) of 1990 requires health care facilities receiving Medicare or Medicaid funding to inform patients about their rights to create advance directives. State laws vary in terms of the specific requirements for creating a valid advance health care directive. To create a valid advance health care directive, individuals generally need to meet the following criteria: Age and mental capacity: The person creating the directive must be at least 18 years old and have the mental capacity to understand the document's purpose and implications. Witnesses and notarization: Most states require that advance health care directives be signed in the presence of witnesses or a notary public to ensure their validity. Proper documentation: Advance health care directives must be documented using state-approved forms or language that meets the legal requirements of the jurisdiction. A living will is a type of advance health care directive that outlines an individual's preferences for medical treatment in specific situations, such as terminal illness, persistent vegetative state, or severe brain injury. In a living will, individuals can specify their wishes regarding life-sustaining treatments, such as artificial nutrition and hydration, ventilator support, and cardiopulmonary resuscitation (CPR). Living wills may not cover all possible medical situations, and their interpretation may be subject to ambiguity. Additionally, living wills only apply when a person is unable to communicate their wishes and make decisions for themselves. A durable power of attorney for health care, also known as a health care proxy or medical power of attorney, allows an individual to designate a trusted person, known as a health care agent, to make medical decisions on their behalf if they become incapacitated. When appointing a healthcare agent, it is essential to choose someone who understands the individual's values and preferences and is willing to advocate on their behalf. The health care agent's authority can be broad or limited, depending on the language used in the document. However, certain decisions, such as those involving experimental treatments or withdrawal of life-sustaining measures, may be subject to specific legal requirements or limitations. A Do Not Resuscitate (DNR) order is a medical order that instructs health care providers not to perform CPR in the event of cardiac or respiratory arrest. DNR orders are typically issued by a physician, often in consultation with the patient or their legally authorized representative, and included in the patient's medical record. DNR orders only apply to CPR and do not address other life-sustaining treatments or medical interventions. When creating an advance health care directive, it is important to consider one's values, beliefs, and preferences regarding medical treatments, quality of life, and end-of-life care. These factors should guide the choices made in the document. Discussing one's wishes and preferences with family members and health care providers is essential to ensure that they understand and are prepared to honor the advance health care directive. Open communication can help prevent misunderstandings and conflicts during a medical crisis. Advance health care directives should be reviewed and updated regularly, particularly when there are significant changes in one's health status, personal relationships, or medical preferences. Keeping the document current helps ensure that it accurately reflects the individual's wishes. Advance health care directives should be stored in a safe yet accessible location, and copies should be provided to family members, health care agents, and primary care physicians. In some states, advance directives can also be registered in a central database to facilitate access by health care providers. Advance health care directives promote patient autonomy by allowing individuals to express their preferences for medical care. However, this can sometimes conflict with the principle of paternalism, where health care providers may feel obligated to act in the best interest of the patient, even if it contradicts the patient's wishes. Different cultural, religious, and moral perspectives can influence individuals' views on advance health care directives and end-of-life care. It is important to be sensitive to these differences and ensure that the advance directive is consistent with the individual's beliefs and values. Advance health care directives can sometimes lead to conflicts among family members or health care providers, particularly when there is disagreement about the interpretation of the document or the appropriateness of specific medical interventions. Resolving these conflicts may require mediation, legal intervention, or the involvement of an ethics committee. Advance health care directives play a critical role in promoting autonomy and quality of life for patients who are unable to communicate or make decisions for themselves. Creating an advance health care directive can provide peace of mind for individuals and their families, ensuring that their preferences are respected during difficult times. By fostering ongoing education and awareness efforts, society can better understand and utilize advance health care directives to improve patient care and uphold individual autonomy.What Are Advance Health Care Directives?
Legal Framework and Requirements
Federal and State Laws
Requirements for a Valid Advance Health Care Directive
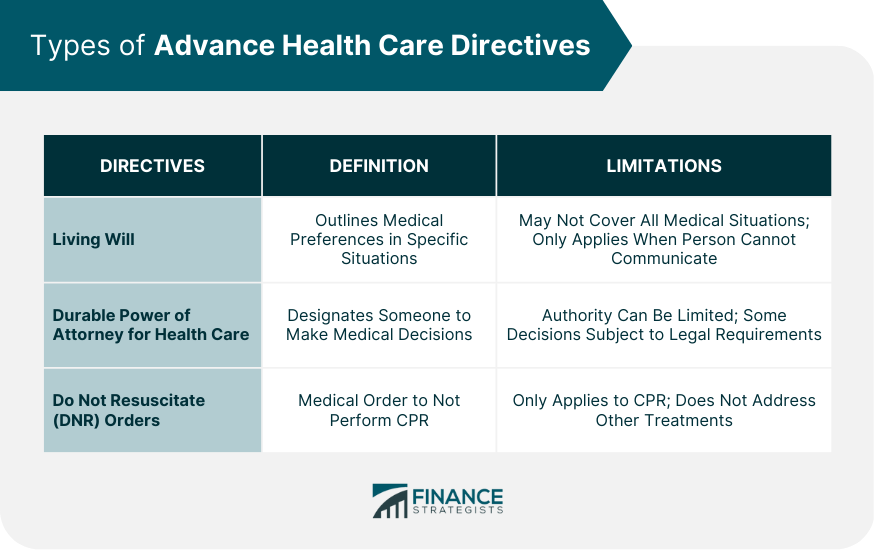
Types of Advance Health Care Directives
Living Will
Definition and Purpose
Specifying Treatment Preferences
Limitations
Durable Power of Attorney for Health Care
Definition and Purpose
Appointment of a Health Care Agent
Scope of Authority and Limitations
Do Not Resuscitate (DNR) Orders
Definition and Purpose
Implementation Process
Limitations
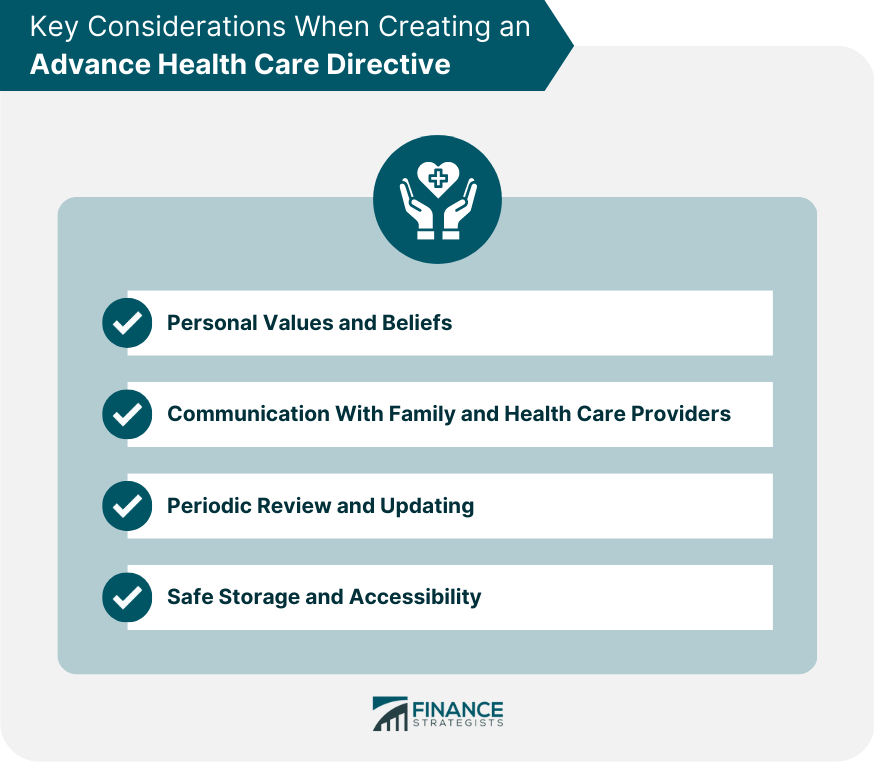
Key Considerations When Creating an Advance Health Care Directive
Personal Values and Beliefs
Communication With Family and Health Care Providers
Periodic Review and Updating
Safe Storage and Accessibility
Ethical Issues Surrounding Advance Health Care Directives
Autonomy vs Paternalism in Medical Decision-Making
Cultural, Religious, and Moral Perspectives
Potential Conflicts Among Family Members or Health Care Providers
Conclusion
Advance Health Care Directives FAQs
An advance healthcare directive is a legal document that specifies your medical treatment preferences and appoints a healthcare proxy to make decisions on your behalf in case you become unable to communicate your wishes.
An advance healthcare directive ensures that your medical treatment preferences are respected and followed, even if you are unable to communicate them. It also helps avoid potential conflicts among family members about your medical care.
Anyone over the age of 18 should have an advance healthcare directive, regardless of their current health status. Unexpected medical emergencies can happen to anyone at any time, so it's important to be prepared.
Yes, you can change your advance healthcare directive at any time, as long as you are still competent to make decisions. You should review and update your directive regularly, especially if your health status or treatment preferences change.
You can create an advance healthcare directive by consulting with an attorney or using an online template. You should also discuss your medical treatment preferences with your healthcare provider and your chosen healthcare proxy, to ensure that your wishes are understood and followed.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











