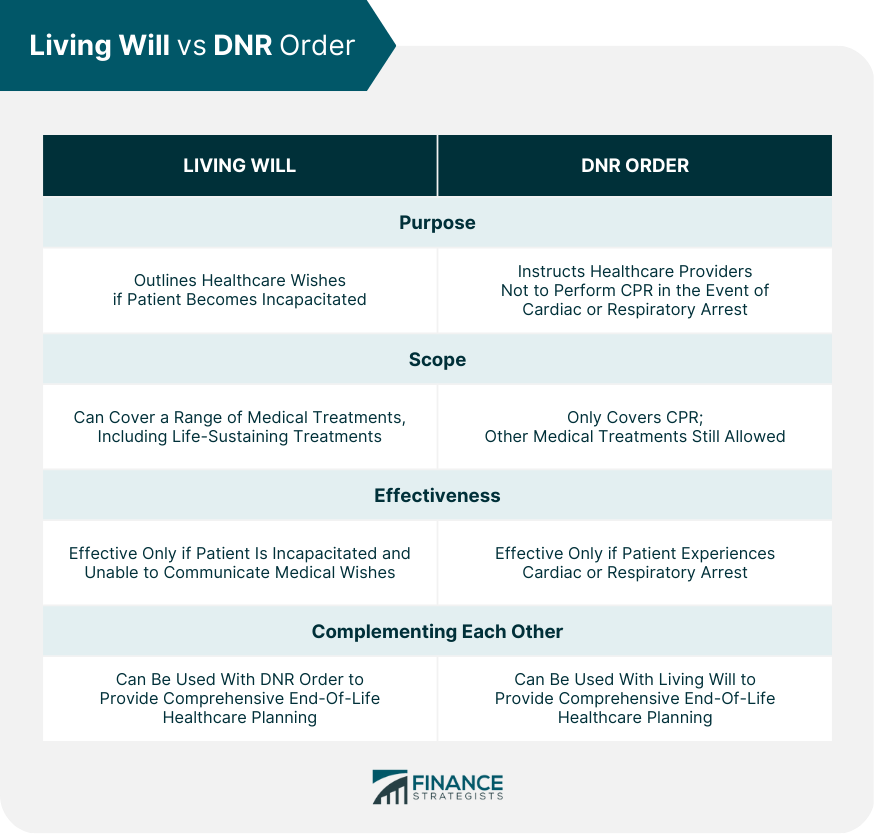
Living wills and DNRs or Do-Not-Resuscitate orders are important legal documents for end-of-life healthcare planning. A living will specifies a person's healthcare wishes in the event they become incapacitated. On the other hand, a DNR instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. Both documents can be used together to provide comprehensive end-of-life healthcare planning. It is important to understand each document's legal requirements and potential consequences and to discuss your wishes with your loved ones and healthcare providers. Regularly reviewing and updating your living will and DNR ensures that they reflect your current wishes. A living will is a legal document that outlines a person's healthcare wishes if they cannot communicate them. This document allows patients to express their desires regarding medical treatment, including life-sustaining treatments, such as artificial hydration and nutrition, mechanical ventilation, and resuscitation. Living wills are also called advance directives, medical directives, or healthcare declarations. Living wills ensure that patients receive medical treatment per their wishes, even if they are incapacitated. In essence, it allows individuals to have control over their medical treatment even if they cannot communicate their wishes. A living will is only effective if the patient is incapacitated and unable to communicate their medical wishes. If the patient is still able to communicate, it has no effect. By having a living will in place, patients can ensure that their medical treatment aligns with their values and preferences. A DNR is a medical order that instructs healthcare providers not to perform CPR in the event of cardiac or respiratory arrest. Patients with terminal illnesses, chronic medical conditions, or at the end stages of life typically request this order. CPR involves using chest compressions, rescue breaths, and defibrillation to restart the heart and lungs. DNR orders are designed to ensure patients do not receive unwanted medical treatment that could cause discomfort or pain. They also prevent unnecessary medical interventions that could prolong the dying process. DNR orders are only effective if a patient experiences cardiac or respiratory arrest. If a patient can still communicate, the DNR order has no effect. Living wills and DNR orders are two types of advance directives that are used in end-of-life healthcare planning. While they may seem similar, there are important differences between these two documents. Here is a more detailed explanation of the key differences: A living will outlines a patient's healthcare wishes in the event they become incapacitated. It covers a range of medical treatments and procedures that the patient may or may not want to receive. This includes life-sustaining treatments such as artificial hydration and nutrition, mechanical ventilation, and resuscitation. A living will is intended to help healthcare providers make decisions about medical treatments when the patient is unable to communicate their wishes. On the other hand, a DNR order instructs healthcare providers not to perform CPR in the event of cardiac or respiratory arrest. This means that if the patient's heart stops beating or they stop breathing, healthcare providers will not attempt to revive them with CPR. Living wills cover a range of medical treatments and procedures, while DNR orders only cover CPR. Other medical treatments, such as intubation, medication administration, and transfusions, are still allowed if the patient's heart is still beating and they are still breathing. A living will is only effective if the patient is incapacitated and unable to communicate their medical wishes. This means that healthcare providers will look to the living will to determine what treatments to provide or withhold. A DNR order, on the other hand, is only effective if the patient experiences cardiac or respiratory arrest. Healthcare providers will follow the DNR order and not attempt to perform CPR if such an event occurs. While living wills and DNR orders have different purposes and scopes, they can complement each other to provide comprehensive end-of-life healthcare planning. A living will can help guide medical treatment decisions before a cardiac or respiratory arrest occurs, while a DNR order is in effect only if such an event occurs. Both a living will and a DNR order can be used together to ensure that a patient's healthcare wishes are respected and followed in all circumstances. For example, if a patient does not want to receive CPR but would like to receive other medical treatments, a living will and a DNR order can both be used to communicate these preferences to healthcare providers. When creating a living will or DNR order, it is important to consider each document's legal requirements and potential consequences. In the United States, each state has its own laws governing living wills and DNR orders. It is important to research the laws in your state to ensure that your documents are legally binding. When creating a living will, it is important to specify your healthcare wishes in clear and specific terms. Your healthcare providers will use this document as a guide when making medical treatment decisions on your behalf. If your wishes need to be clarified or clarified, it may be difficult for healthcare providers to follow them. Similarly, when creating a DNR order, it is important to ensure that a qualified medical professional signs it and that it is included in your medical records. This ensures that your healthcare providers are aware of your wishes and can follow them in the event of a cardiac or respiratory arrest. Discussing your healthcare wishes with your family and loved ones is also important. This ensures they know your desires and can advocate on your behalf if necessary. In addition, it is important to review and update your Living Will and DNR order regularly to ensure that they continue to reflect your wishes. Living wills and DNR orders are essential legal documents for end-of-life healthcare planning. While a living will specifies a person's healthcare wishes if they become incapacitated, a DNR order instructs healthcare providers not to perform CPR in the event of cardiac or respiratory arrest. Both documents complement each other to provide comprehensive end-of-life healthcare planning. It is crucial to understand each document's legal requirements and potential consequences and to discuss your wishes with your family and healthcare providers. Regularly reviewing and updating your living will and DNR order ensures they reflect your current wishes. Planning for end-of-life healthcare can be a complex and emotional process, and it is important to seek help from professionals. An estate planning lawyer can provide guidance and support in creating a comprehensive end-of-life healthcare plan that aligns with your values and financial goals. Living Will vs DNR: An Overview
What Is a Living Will?
What Is a DNR?
Living Will vs DNR: Key Differences
Purpose
Scope
Effectiveness
Complementing Each Other
Living Will vs DNR Legal Considerations
Conclusion
Living Will vs DNR FAQs
A living will specifies a person's healthcare wishes if they become incapacitated and cannot communicate them to their healthcare providers.
A DNR order instructs healthcare providers not to perform CPR in the event of cardiac or respiratory arrest, ensuring that patients do not receive unwanted medical treatment that could cause discomfort or pain.
Yes, a living will and a DNR order can be used together to provide comprehensive end-of-life healthcare planning. A living will can guide medical treatment decisions before a cardiac or respiratory arrest occurs, while a DNR order is in effect only if such an event occurs.
Yes, Living Wills and DNR orders are legally binding documents in the United States, and each state has its laws governing them. It is important to research the laws in your state to ensure that your documents are legally binding.
Discussing living wills and DNRs with healthcare providers and loved ones ensures that your wishes are known and can be respected. It can also help to avoid confusion or disagreement among family members during difficult times.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











