The Health Insurance Portability and Accountability Act (HIPAA) is a United States federal law enacted in 1996 that aims to protect the privacy and security of patient health information and improve the efficiency of the healthcare system. HIPAA was established to address growing concerns about the confidentiality of patient health information in an increasingly digital age. Its primary goals are to ensure the portability of health insurance coverage, safeguard patient privacy, and standardize electronic healthcare transactions. HIPAA is composed of two main titles: Title I, which focuses on health insurance portability, and Title II, which deals with administrative simplification, including privacy and security rules, as well as transaction and code set standards. HIPAA limits the extent to which group health plans can impose pre-existing condition exclusions, ensuring that individuals with pre-existing health conditions can maintain their insurance coverage when transitioning between jobs or health plans. Under HIPAA, group health plans are required to provide special enrollment opportunities for eligible individuals experiencing qualifying life events, such as marriage or the birth of a child. This ensures continuous health insurance coverage for individuals and their dependents. HIPAA works in conjunction with the Consolidated Omnibus Budget Reconciliation Act (COBRA) to ensure that individuals who lose their job-based health insurance can continue their coverage for a limited period, maintaining their access to healthcare services. The HIPAA Privacy Rule establishes standards for the protection of Protected Health Information, which includes any identifiable health information held or transmitted by a covered entity or its business associate in any form or media, whether electronic, paper, or oral. Under the Privacy Rule, covered entities must implement privacy policies and procedures, limit the use and disclosure of PHI, and provide individuals with access to their health information. Additionally, covered entities must provide a Notice of Privacy Practices to patients, explaining how their information is used and disclosed. The HIPAA Security Rule requires covered entities to implement administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of electronic PHI (ePHI). These safeguards include access controls, workforce training, and facility security measures. To comply with the Security Rule, covered entities must conduct regular risk assessments to identify potential threats and vulnerabilities to ePHI. They must also implement a risk management process to mitigate identified risks, ensuring the ongoing protection of sensitive health information. The Transactions and Code Sets Rule establishes standard formats for electronic healthcare transactions, such as claims, eligibility inquiries, and payment remittance advice. This standardization simplifies and streamlines the exchange of information between healthcare providers, payers, and other stakeholders. The HIPAA Transactions and Code Sets Rule also requires the use of standardized code sets for diagnoses, procedures, and drugs, as well as unique identifiers for providers, employers, and health plans. These standards promote efficiency and consistency in the processing and exchange of healthcare data. The Office for Civil Rights is responsible for enforcing HIPAA's Privacy and Security Rules. OCR investigates complaints, conducts compliance reviews, and provides guidance to help covered entities understand and comply with the regulations. HIPAA violations can result in significant civil and criminal penalties, ranging from monetary fines to imprisonment, depending on the nature and severity of the violation. Penalties aim to deter noncompliance and ensure the protection of patient's health information. OCR conducts compliance audits and investigations to assess covered entities' adherence to HIPAA regulations. These audits evaluate an organization's policies, procedures, and safeguards, identifying areas for improvement and ensuring compliance with the Privacy and Security Rules. HIPAA has greatly enhanced patient privacy and confidentiality by establishing strict standards for the use, disclosure, and protection of health information. This has increased patients' trust in the healthcare system and encouraged them to seek necessary care without fear of privacy breaches. HIPAA has facilitated the adoption and use of EHRs and promoted secure data exchange between healthcare providers, payers, and other stakeholders. This has improved care coordination, reduced medical errors, and enhanced the overall quality of care. By standardizing electronic transactions and code sets, HIPAA has streamlined administrative processes, reduced paperwork, and increased efficiency within the healthcare industry. These improvements have led to cost savings for providers, payers, and patients. Implementing and maintaining HIPAA-compliant systems can be complex and resource-intensive, requiring ongoing updates, staff training, and monitoring. As technology evolves, covered entities must adapt to new security threats and ensure continued compliance with HIPAA regulations. Health Information Technology plays a crucial role in helping covered entities achieve HIPAA compliance. HIT solutions, such as EHRs and secure messaging platforms, incorporate built-in privacy and security features that facilitate the protection of sensitive health information. Emerging technologies, such as artificial intelligence, telemedicine, and blockchain, have the potential to transform the healthcare industry while posing new challenges for HIPAA compliance. Covered entities must remain vigilant in adapting their privacy and security practices to address these evolving technologies. HIPAA has been instrumental in protecting patient privacy, promoting the secure exchange of health information, and improving healthcare efficiency. By establishing robust privacy and security standards, HIPAA has fostered trust in the healthcare system and facilitated the adoption of innovative health technologies. Despite the progress made in implementing HIPAA, ongoing challenges remain in maintaining compliance and addressing emerging threats to patient privacy. Covered entities must continue to invest in staff training, technology, and security measures to ensure the protection of health information. As technology and the healthcare landscape continue to evolve, HIPAA will remain a critical regulatory framework for safeguarding patient privacy and promoting efficient, high-quality care. Ongoing vigilance, innovation, and collaboration among stakeholders will be essential in adapting HIPAA to the changing needs of the healthcare industry.What Is the Health Insurance Portability and Accountability Act (HIPAA)?
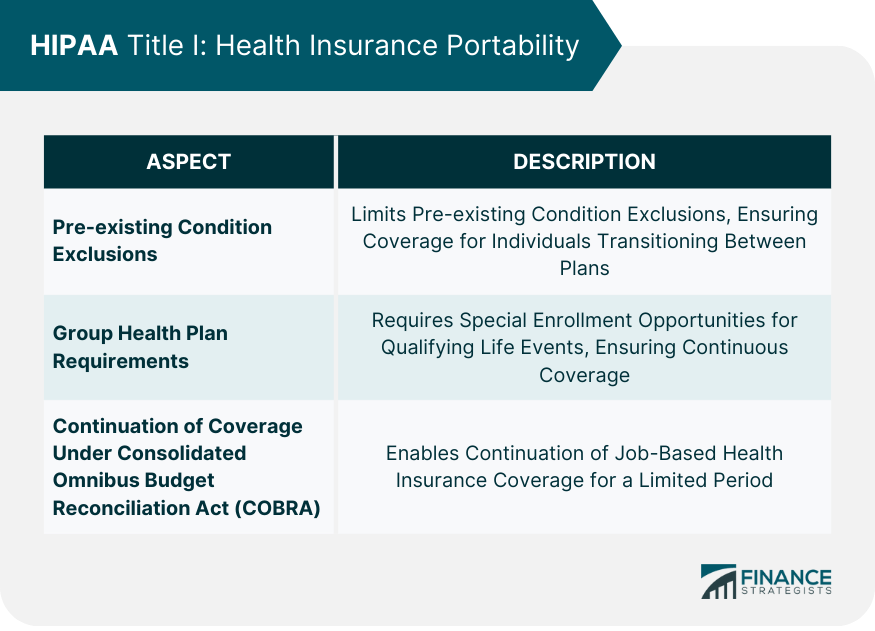
HIPAA Title I: Health Insurance Portability
Pre-existing Condition Exclusions
Group Health Plan Requirements
Continuation of Coverage Under COBRA
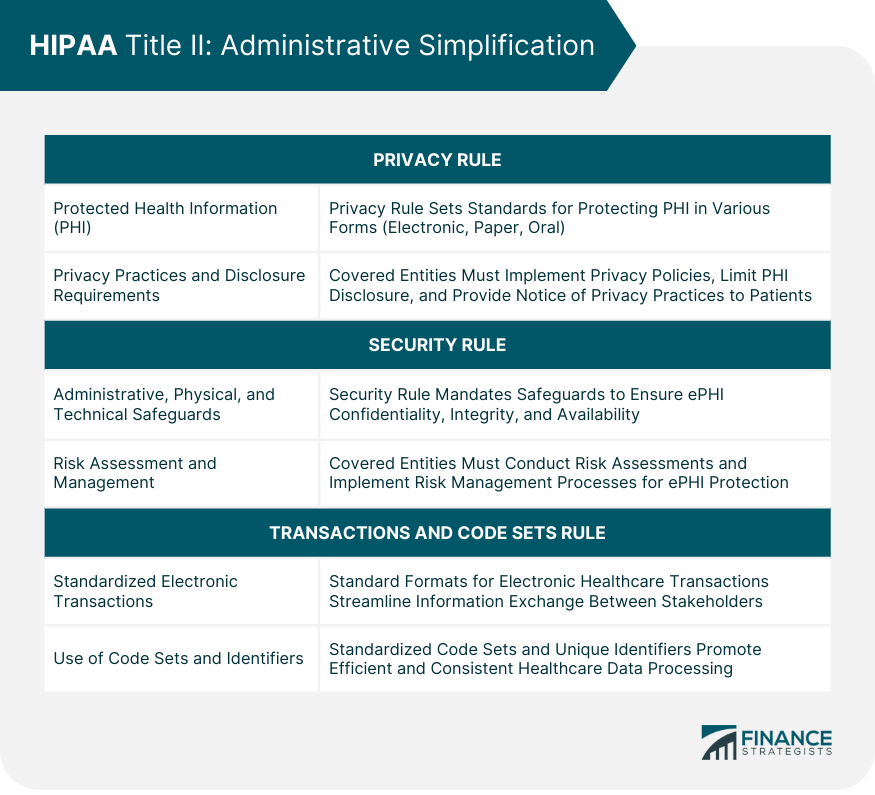
HIPAA Title II: Administrative Simplification
Privacy Rule
Protected Health Information (PHI)
Privacy Practices and Disclosure Requirements
Security Rule
Administrative, Physical, and Technical Safeguards
Risk Assessment and Management
Transactions and Code Sets Rule
Standardized Electronic Transactions
Use of Code Sets and Identifiers
Enforcement of HIPAA
Office for Civil Rights (OCR) Role
HIPAA Violations and Penalties
Compliance Audits and Investigations
Impact of HIPAA on the Healthcare Industry
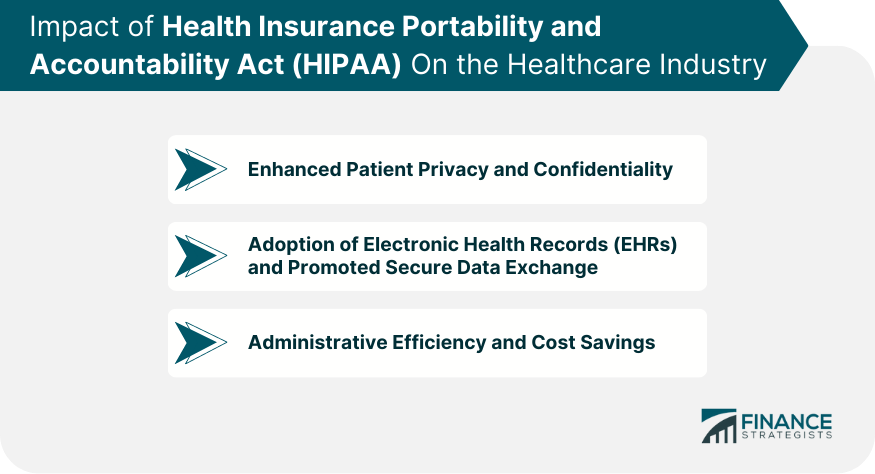
Patient Privacy and Confidentiality
Electronic Health Records (EHRs) and Data Exchange
Administrative Efficiency and Cost Savings
HIPAA and Technology
Challenges of Implementing and Maintaining HIPAA-Compliant Systems
Role of Health Information Technology (HIT) in Compliance
Emerging Technologies and Their Impact on HIPAA
Final Thoughts
Health Insurance Portability and Accountability Act (HIPAA) FAQs
HIPAA is a United States federal law enacted in 1996 with the primary purpose of protecting the privacy and security of patient health information and improving the efficiency of the healthcare system. It ensures health insurance portability and establishes standards for the use, disclosure, and protection of health information.
HIPAA's Privacy Rule establishes standards for the protection of Protected Health Information (PHI), which includes any identifiable health information held or transmitted by a covered entity or its business associate. Covered entities must implement privacy policies and procedures, limit the use and disclosure of PHI, and provide individuals with access to their health information.
HIPAA violations can result in significant civil and criminal penalties, depending on the nature and severity of the violation. Penalties range from monetary fines to imprisonment and aim to deter noncompliance and ensure the protection of patient's health information.
HIPAA has facilitated the adoption and use of Electronic Health Records (EHRs) and promoted secure data exchange between healthcare providers, payers, and other stakeholders. It has improved care coordination, reduced medical errors, and enhanced the overall quality of care by standardizing electronic transactions and code sets.
Implementing and maintaining HIPAA-compliant systems can be complex and resource-intensive. Covered entities must navigate ongoing updates, staff training, and monitoring to ensure compliance with HIPAA regulations. As technology evolves, organizations must adapt to new security threats and maintain continuous compliance.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











