Before the Affordable Care Act's inception, Medicaid acted as the primary safety net for numerous low-income individuals, especially those belonging to vulnerable groups. The ACA ushered in significant changes, offering a chance for states to cover a wider segment of their low-income population. It introduced clearer eligibility based on household income, seeking to include those who were previously overlooked. This meant households with incomes up to 138% of the federal poverty level could access medical coverage. This expansion aimed to reduce disparities and make health coverage more inclusive. The Medicaid expansion through the ACA aimed at a major goal: reducing the number of uninsured Americans. The traditional Medicaid structure left several adults, particularly those without dependent children, in a tricky situation. They earned too much for Medicaid but couldn’t afford private insurance. The ACA’s Medicaid expansion sought to bridge this gap. By ensuring more people could access health services, the nation's overall health prospects were set to improve. The expectation was that with better health coverage, citizens would lead healthier lives, leading to long-term societal benefits. The application became more user-friendly, with online platforms guiding applicants. Once the necessary income details were submitted and verified, the system determined eligibility. Continual checks ensured beneficiaries remained qualified for the benefits they received. Medicaid is jointly funded by federal and state governments. The ACA’s expansion meant the federal government would foot a large chunk of the bill for new enrollees. However, this brought about concerns. Would states be able to manage if the federal commitment waned? Such uncertainties presented financial challenges for state policymakers. ACA’s Medicaid expansion wasn't just about numbers; it aimed at offering comprehensive services. Beneficiaries received a range of essential health benefits, from outpatient care to mental health services. Additionally, preventive services, crucial for early detection of potential health issues, became available at no extra cost. This forward-thinking approach aims to manage health problems before they become severe and more costly. The ACA’s Medicaid expansion led to a marked increase in insured Americans. By making eligibility more inclusive, many found themselves newly eligible for medical coverage. The ACA aimed at creating uniformity across states in terms of health coverage, making access more equitable. Economic advantages of Medicaid expansion were manifold. Hospitals, previously burdened with unpaid care costs, saw a significant reduction as more patients gained insurance. This lightened the financial load and improved healthcare delivery. On a broader scale, states that expanded Medicaid reaped economic benefits. With federal funds covering a significant portion of Medicaid costs, states could allocate resources to other areas, spurring economic growth and potentially creating new job opportunities. Improved health outcomes stood out as a hallmark of Medicaid expansion. Access to timely medical services meant that conditions could be diagnosed and treated earlier. There were indications of a correlation between the expansion and reduced mortality rates. A population with better access to healthcare could lead to a healthier society, showcasing the long-term vision of the ACA. While the ACA promised substantial federal support, states faced the challenge of funding their share of Medicaid. Any increase in state spending had to be balanced against other priorities. Additionally, states had to contend with the unpredictability of future federal support, causing concerns over long-term sustainability. Different states had varied responses to Medicaid expansion, leading to diverse administrative challenges. Some states, while enthusiastic, faced hurdles in effective implementation. The surge in beneficiaries meant health departments had to process a larger volume of applications, sometimes leading to administrative delays. More insured individuals meant a higher demand for health services. In areas where healthcare providers were already scarce, this increased demand posed challenges. Not all doctors were willing to accept Medicaid patients, given the lower reimbursements compared to private insurance. This discrepancy could lead to longer wait times, potentially negating the benefits of expanded coverage. Many states opted for Medicaid expansion, understanding the potential benefits for their citizens. In these states, uninsured rates decreased substantially, and the financial health of hospitals improved. However, the path to expansion varied. Some states took phased approaches, while others sought federal waivers to tailor the expansion to their specific conditions. Several states chose not to expand Medicaid. Their reasons ranged from financial concerns to differing opinions on the ACA’s principles. These states didn't see the same dip in uninsured rates as their expanding counterparts. The coverage gap, where individuals earned too much for traditional Medicaid but not enough for ACA marketplace subsidies, was more pronounced in these states. States' decisions on Medicaid expansion had significant repercussions. Expansion states saw uninsured rates plummet, bringing in societal and economic advantages. Conversely, non-expanding states had higher uninsured rates, and their hospitals faced more financial strain from unpaid care. Over time, health and financial disparities between these two groups of states could become even more pronounced. Medicaid expansion became a central talking point in political circles. Politicians either lauded it as a pivotal move towards comprehensive healthcare or criticized it as an example of federal excess. These partisan debates influenced state decisions, overshadowing objective evaluation of the policy. Media portrayal, political leanings, and personal experiences molded public opinion on Medicaid expansion. Unfortunately, this often led to misconceptions. Many eligible individuals missed out simply because they weren't aware or had false beliefs about their qualifications. Medicaid expansion was not without its long-term concerns. How would states manage if federal support waned? And could the system handle the increasing number of beneficiaries in the future? The ACA's Medicaid expansion's sustainability remains a topic of debate, requiring constant observation and potential adjustments. Medicaid expansion under the Affordable Care Act marked a significant shift in the U.S. healthcare landscape, aiming to make health coverage more inclusive. By broadening eligibility, millions found themselves with newfound access to vital health services. While the initiative ushered in economic benefits and improved health outcomes, states grappled with financial uncertainties and administrative challenges. The divide between states that embraced the expansion and those that refrained created disparities in uninsured rates and the financial health of their healthcare institutions. Public opinion remained divided, influenced by political debates and, at times, misinformation. As the nation moves forward, the long-term sustainability of ACA's Medicaid expansion will be central to discussions, underscoring the importance of continual assessment and adaptation.What Is ACA's Medicaid Expansion?
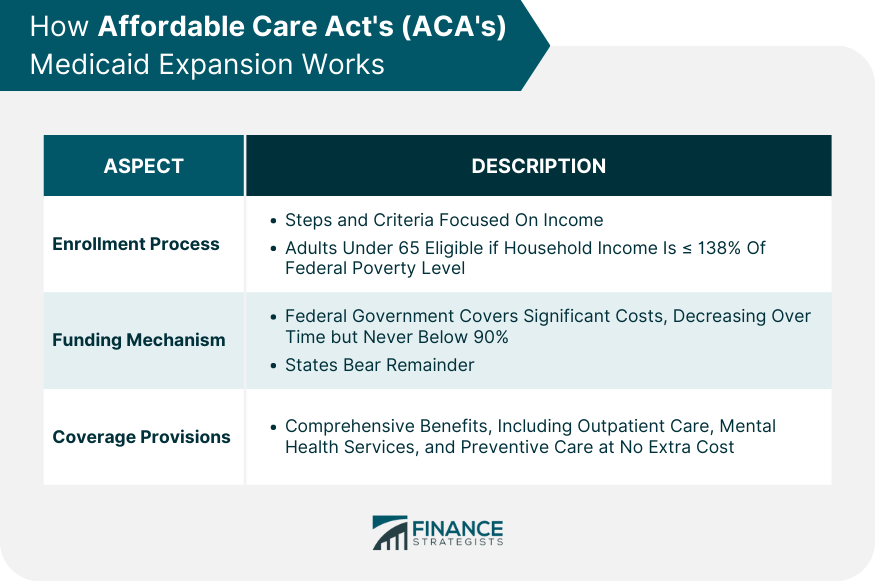
How ACA's Medicaid Expansion Works
Enrollment Process
Funding Mechanism
Coverage Provisions
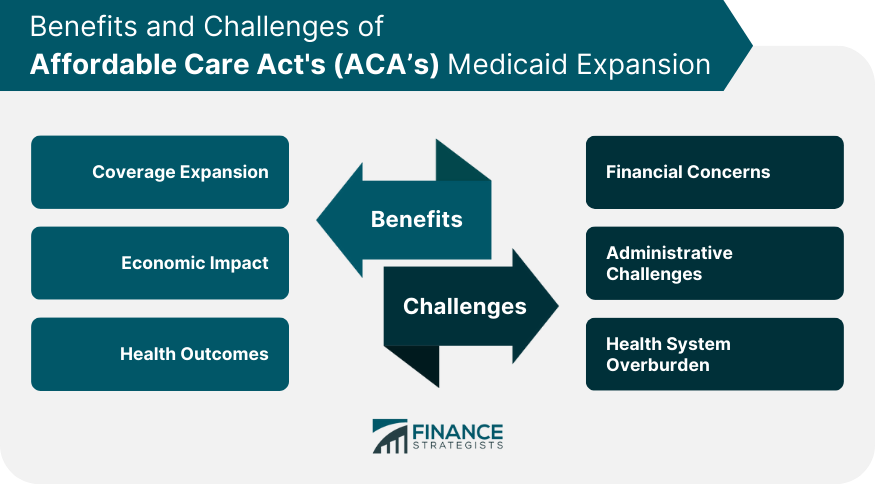
Pros of ACA's Medicaid Expansion
Coverage Expansion
Economic Impact
Health Outcomes
Challenges of ACA's Medicaid Expansion
Financial Concerns
Administrative Challenges
Health System Overburden
State Decisions on ACA's Medicaid Expansion
States That Embraced Expansion
States That Declined Expansion
Impact on Uninsured Rates and Fiscal Health of States
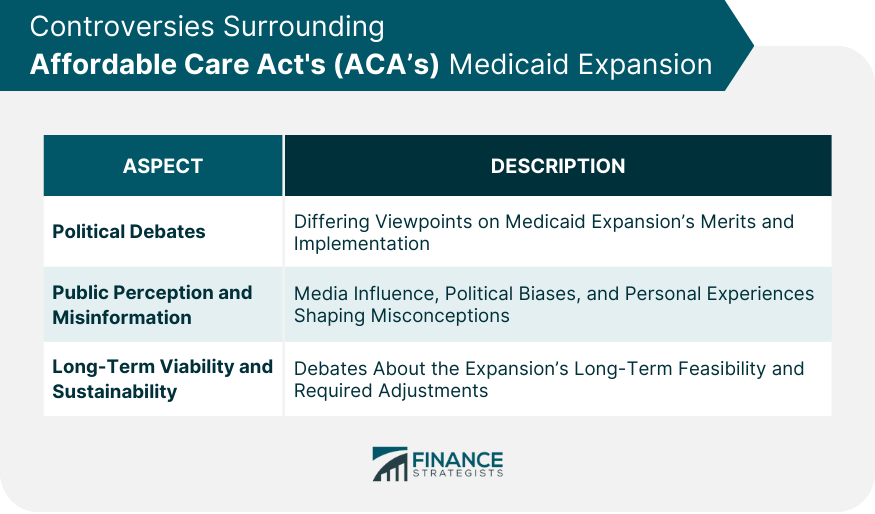
Controversies Surrounding ACA's Medicaid Expansion
Political Debates
Public Perception and Misinformation
Long-Term Viability and Sustainability
Conclusion
Affordable Care Act's (ACA) Medicaid FAQs
The ACA's Medicaid expansion is a provision that broadened Medicaid eligibility to include more low-income adults, specifically those with household incomes at or below 138% of the federal poverty level.
The ACA's Medicaid primarily differs in its expanded eligibility criteria, covering more low-income adults, while traditional Medicaid focuses more on specific groups like children, pregnant women, and the elderly.
Majority of states have adopted the ACA's Medicaid expansion, but the specific list can change. It's recommended to check the current state's health department website or the Centers for Medicare & Medicaid Services for the latest information.
The ACA's Medicaid expansion brought economic benefits, like decreased uncompensated care costs for hospitals and increased federal funding for states that adopted the expansion. However, concerns about long-term funding sustainability persist.
Yes, the ACA's Medicaid expansion has been a topic of political debate, with opinions divided on its merits and long-term viability. Factors like state decisions on adoption, public perception, and questions of financial sustainability have fueled these controversies.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











