Medicaid is a government-sponsored health insurance program in the United States, designed to provide affordable healthcare to eligible low-income individuals and families. Established in 1965, Medicaid is jointly funded by federal and state governments and administered by individual states. Eligibility for Medicaid is determined by various factors, including income, age, disability, and family status. Although each state has its own specific eligibility rules, there are federal guidelines that states must follow to ensure coverage for certain populations. Inpatient hospital services include medical care that requires overnight stays at a hospital. Medicaid covers these services for eligible beneficiaries, ensuring they receive necessary care for conditions requiring hospitalization. Medicaid also covers nursing and other services necessary for the proper treatment of the beneficiary during their hospital stay. This includes meals, medications, and rehabilitation services, if required. Outpatient hospital services encompass medical care that does not require an overnight stay in a hospital, such as diagnostic tests, emergency care, and preventive care. Medicaid covers these services to ensure beneficiaries have access to essential healthcare without incurring excessive costs. Some states may limit the number of outpatient services covered by Medicaid, but federal law mandates that states must provide certain outpatient services, such as family planning and federally qualified health center services. Medicaid covers physician services to ensure beneficiaries receive appropriate care from qualified medical professionals. This includes consultations, diagnoses, treatment, and preventive care provided by licensed doctors, whether in a hospital or clinic setting. In some cases, Medicaid also covers the services of other healthcare providers, such as nurse practitioners, who work under the supervision of a physician. This ensures that beneficiaries receive comprehensive care from a wide range of healthcare professionals. Nursing facility services are covered by Medicaid for eligible beneficiaries who require long-term care in a skilled nursing facility. These services include room and board, nursing care, rehabilitation services, and medical supplies. Medicaid also covers intermediate care facilities for individuals with intellectual disabilities, providing specialized care and support for those who require assistance with daily living activities and ongoing medical supervision. Home health services provide medical care and support to eligible beneficiaries in their own homes, allowing them to maintain their independence and avoid institutionalization. Medicaid covers a range of home health services, including skilled nursing care, home health aide services, and medical supplies. In some cases, Medicaid may also cover personal care services for beneficiaries who require assistance with daily living activities, such as bathing, dressing, and meal preparation. These services aim to improve beneficiaries' quality of life and support their overall well-being. Medicaid covers laboratory and X-ray services to ensure beneficiaries have access to essential diagnostic tests and screenings. These services play a crucial role in the early detection, diagnosis, and treatment of various medical conditions. Coverage of these services may vary by state, but federal law requires states to cover certain laboratory and X-ray services, such as prenatal and pediatric screenings, as well as testing for specific diseases and conditions. The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program provides comprehensive preventive and diagnostic services for Medicaid-eligible children and adolescents under the age of 21. These services aim to identify and treat physical, mental, and developmental issues as early as possible, promoting optimal health and well-being. EPSDT services include regular health screenings, immunizations, dental care, vision care, hearing services, and any necessary diagnostic and treatment services to address identified conditions. Medicaid covers family planning services to help beneficiaries make informed decisions about their reproductive health and family size. These services include counseling, education, and access to contraceptive methods, as well as testing and treatment for sexually transmitted infections. Family planning services also cover pregnancy-related care, including prenatal care, labor and delivery services, and postpartum care. By covering these services, Medicaid helps to promote healthy pregnancies and positive birth outcomes for beneficiaries. Rural health clinic services are essential for Medicaid beneficiaries who live in rural areas with limited access to healthcare providers. Medicaid covers these services, ensuring that rural residents can access necessary primary care, diagnostic, and preventive services. These clinics often provide care through a team of healthcare professionals, including physicians, nurse practitioners, and physician assistants. This team-based approach ensures that rural beneficiaries receive comprehensive and coordinated care, addressing their unique healthcare needs. Federally Qualified Health Center (FQHC) are community-based healthcare providers that offer comprehensive primary care services to medically underserved populations, regardless of their ability to pay. Medicaid covers FQHC services for eligible beneficiaries, ensuring access to affordable and high-quality care. Services provided by FQHCs include primary care, dental care, mental health services, substance use disorder treatment, and preventive health services. By covering these services, Medicaid helps to address health disparities and improve health outcomes for vulnerable populations. While not mandated by federal law, most states opt to provide prescription drug coverage for their Medicaid beneficiaries. This coverage includes access to a wide range of medications, ensuring that beneficiaries can receive the necessary treatments for their medical conditions. Prescription drug coverage may vary by state, and some states may implement cost-sharing measures or restrict coverage to specific drug classes. Despite these limitations, prescription drug coverage remains a crucial component of comprehensive healthcare for Medicaid beneficiaries. Dental services are an optional Medicaid benefit that states can choose to provide for their beneficiaries. While federal law requires states to cover dental services for children under the EPSDT program, adult dental coverage varies significantly by state. Some states offer comprehensive dental coverage for adults, while others may only cover emergency dental services or have limited coverage. Dental services are essential for maintaining overall health and well-being, and access to these services can help prevent more serious and costly health problems. Physical, occupational, and speech therapy services are optional benefits that states can choose to offer their Medicaid beneficiaries. These therapies can help individuals regain function and independence after an injury, illness, or disability. Physical therapy focuses on improving mobility and physical function, occupational therapy addresses daily living skills and adaptive strategies, and speech therapy helps with communication and swallowing difficulties. By covering these services, Medicaid can support beneficiaries in their recovery and rehabilitation process. Personal care services are an optional Medicaid benefit that provides assistance with daily living activities for eligible beneficiaries who require help due to a disability, chronic illness, or age-related decline. These services can include assistance with bathing, dressing, meal preparation, and medication management. By covering personal care services, Medicaid helps to improve the quality of life for beneficiaries who may otherwise struggle to maintain their independence and well-being. These services can also help to delay or prevent the need for institutional care, such as nursing home placement. Hospice care is an optional Medicaid benefit that provides end-of-life care for eligible beneficiaries with a terminal illness. Hospice services focus on providing comfort, pain management, and emotional support for both the individual and their family, rather than curative treatments. Hospice care can be provided in various settings, including the individual's home, a hospice facility, or a hospital. By covering hospice services, Medicaid ensures that beneficiaries have access to compassionate and comprehensive end-of-life care. Case management services are an optional Medicaid benefit designed to help beneficiaries navigate the healthcare system and access necessary services and supports. Case managers work with beneficiaries to develop individualized care plans, coordinate services, and monitor progress towards health goals. By covering case management services, Medicaid helps to ensure that beneficiaries receive comprehensive, coordinated care that addresses their unique needs and promotes better health outcomes. Vision care services are an optional Medicaid benefit that states can choose to provide for their beneficiaries. These services can include eye exams, corrective lenses, and treatments for various eye conditions. While federal law requires states to cover vision care services for children under the EPSDT program, adult vision coverage varies by state. Access to vision care services is essential for maintaining overall health and well-being and can help to prevent more serious and costly health problems. Mental health services are an optional Medicaid benefit that states can choose to provide for their beneficiaries. These services include counseling, therapy, psychiatric evaluations, and medication management for individuals with mental health conditions. By covering mental health services, Medicaid helps to address the significant need for mental healthcare in the United States and ensures that beneficiaries have access to appropriate treatments and supports. Substance use disorder treatment is an optional Medicaid benefit that states can choose to provide for their beneficiaries. These services include detoxification, inpatient and outpatient treatment, counseling, and medication-assisted treatment for individuals struggling with substance use disorders. By covering substance use disorder treatment, Medicaid plays a crucial role in addressing the ongoing opioid crisis and supports beneficiaries in their recovery process. Medicaid provides comprehensive healthcare coverage for pregnant women and newborns, ensuring access to essential prenatal care, labor and delivery services, and postpartum care. These services are crucial for promoting healthy pregnancies and positive birth outcomes. Newborns are automatically eligible for Medicaid coverage if their mother was eligible and enrolled at the time of birth. This ensures that infants receive necessary medical care and preventive services from the very beginning of their lives. Medicaid plays a vital role in providing healthcare coverage for millions of children and adolescents in the United States. Through the EPSDT program, Medicaid ensures that eligible children receive comprehensive preventive and diagnostic services, as well as necessary treatments for identified conditions. By covering a wide range of healthcare services for children and adolescents, Medicaid helps to promote optimal health and well-being and supports the healthy development of future generations. Medicaid is an essential source of healthcare coverage for adults with disabilities, providing access to a wide range of services that address their unique needs. These services include medical care, long-term care, home and community-based services, and supports for daily living activities. By covering these services, Medicaid helps to improve the quality of life for adults with disabilities and supports their independence and community integration. Medicaid provides healthcare coverage for millions of low-income seniors, ensuring access to necessary medical care and long-term care services. For many seniors, Medicaid serves as a supplement to Medicare, covering services not fully covered by Medicare, such as long-term care and prescription drug coverage. By covering these services, Medicaid helps to support the health and well-being of seniors and enables them to age with dignity and independence. The Affordable Care Act (ACA) expanded Medicaid eligibility to include more low-income adults, increasing access to affordable healthcare for millions of Americans. Under the expansion, states can choose to cover adults with incomes up to 138% of the federal poverty level. This expansion has significantly reduced the number of uninsured Americans and has improved access to essential healthcare services for many low-income individuals. Under the ACA, states that choose to expand their Medicaid programs must also provide certain enhanced benefits for their newly eligible beneficiaries. These enhanced benefits include coverage for mental health services, substance use disorder treatment, and preventive services. By offering these enhanced benefits, Medicaid expansion has helped to address significant gaps in healthcare coverage and improve health outcomes for vulnerable populations. Medicaid expansion under the ACA is optional, and states can choose whether or not to participate in the expansion. As of 2024, 41 states and the District of Columbia had adopted the expansion, while 10 states had not. States that have adopted the expansion have seen significant improvements in access to healthcare, reductions in the uninsured rate, and improved health outcomes for their residents. Applying for Medicaid involves submitting an application to the appropriate state agency, providing documentation of income, citizenship, and residency, and meeting specific eligibility requirements. The application process may vary by state, but many states offer online applications, in-person assistance, and telephone support to help individuals navigate the application process. Once an application is submitted, the state agency must determine eligibility and notify the applicant of their decision. If approved, the beneficiary can begin accessing Medicaid-covered services and supports. If an individual disagrees with a decision made by their state Medicaid agency, they have the right to appeal that decision. The appeals process may vary by state, but generally involves submitting a written request for an appeal, providing supporting documentation, and attending a hearing or review with a state agency representative. Medicaid beneficiaries also have the right to file grievances if they are dissatisfied with the quality of care or services they receive. Grievances can be filed with the state Medicaid agency, which will investigate the complaint and take appropriate action. While Medicaid aims to provide affordable healthcare coverage for low-income individuals, some beneficiaries may still be required to pay co-payments or participate in cost-sharing for certain services. Co-payments and cost-sharing requirements can vary by state and may depend on factors such as income, age, and type of service. Federal law sets limits on the amount of co-payments and cost-sharing that can be charged to Medicaid beneficiaries, ensuring that out-of-pocket costs remain affordable and do not create barriers to accessing necessary healthcare services. Despite the significant progress made in expanding access to healthcare through Medicaid, ongoing challenges and controversies remain. These include debates over state participation in Medicaid expansion, funding concerns, and efforts to impose work requirements or other restrictions on beneficiaries. Addressing these challenges will require continued advocacy, research, and policy reform to ensure that Medicaid remains a vital source of healthcare coverage for millions of Americans. As policymakers continue to debate the future of Medicaid, various reforms and improvements have been proposed to enhance the program's effectiveness and sustainability. These proposals include simplifying the application process, expanding access to telehealth services, and increasing support for home and community-based services. By implementing targeted reforms and improvements, Medicaid can continue to evolve and adapt to the changing healthcare landscape, ensuring that eligible beneficiaries have access to the comprehensive and affordable healthcare services they need.Definition of Medicaid Benefits
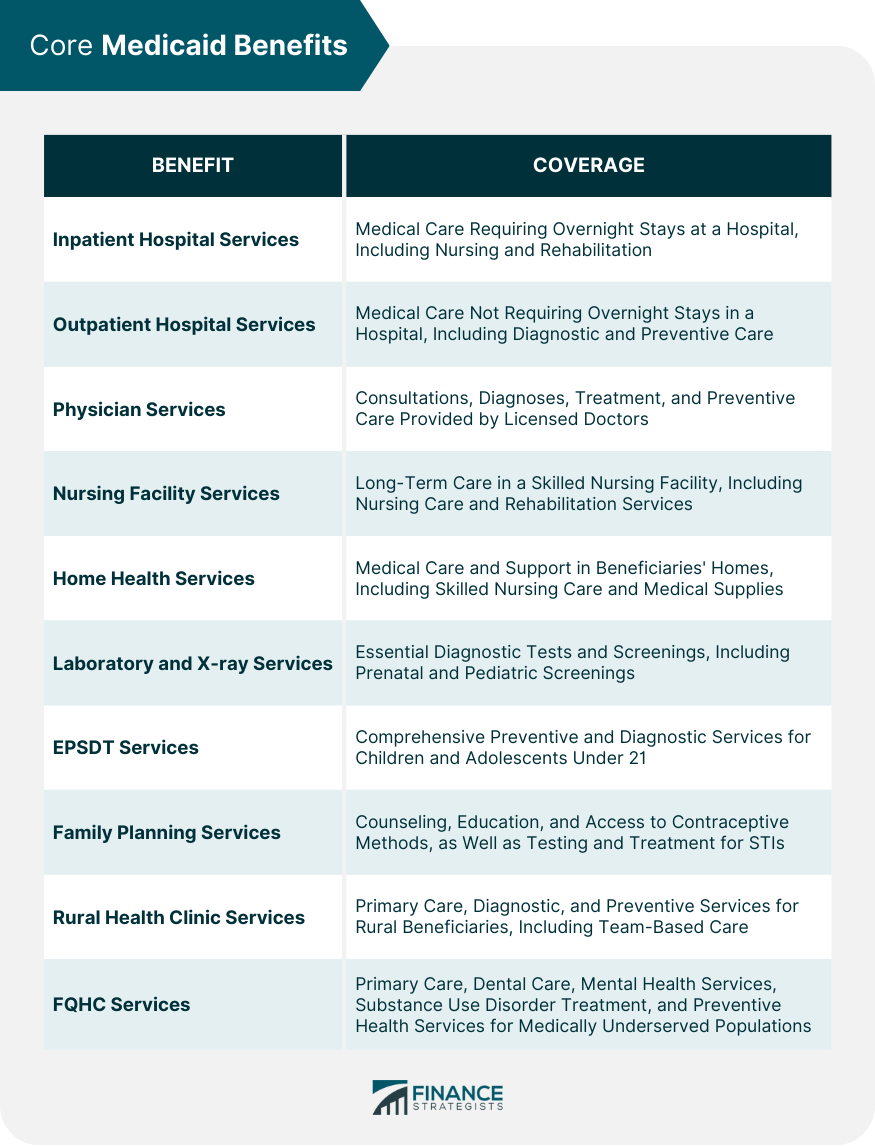
Core Medicaid Benefits
Inpatient Hospital Services
Outpatient Hospital Services
Physician Services
Nursing Facility Services
Home Health Services
Laboratory and X-ray Services
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services
Family Planning Services
Rural Health Clinic Services
Federally Qualified Health Center (FQHC) Services
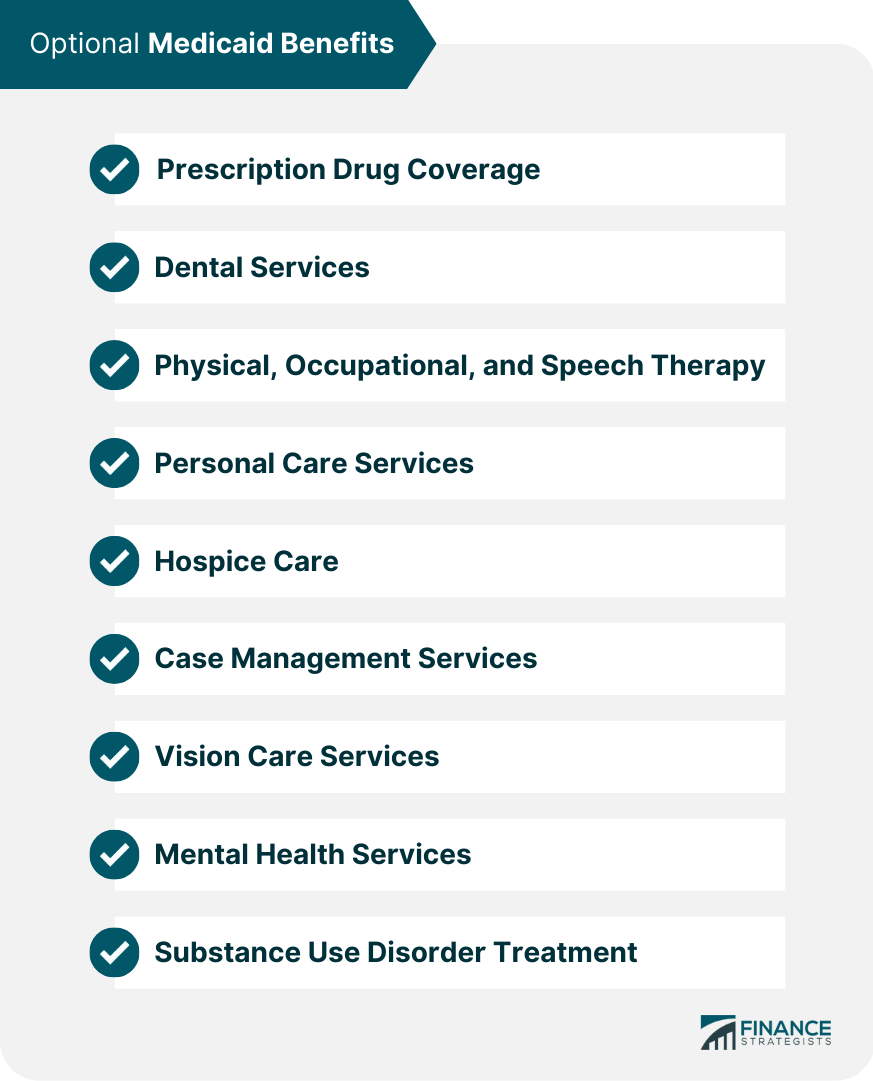
Optional Medicaid Benefits
Prescription Drug Coverage
Dental Services
Physical, Occupational, and Speech Therapy
Personal Care Services
Hospice Care
Case Management Services
Vision Care Services
Mental Health Services
Substance Use Disorder Treatment
Benefits for Specific Populations
Pregnant Women and Newborns
Children and Adolescents
Adults With Disabilities
Seniors
Medicaid Expansion Under the Affordable Care Act (ACA)
Eligibility Expansion
Enhanced Benefits
State Participation
Navigating and Accessing Medicaid Benefits
Application Process
Appeals and Grievances
Co-payments and Cost-Sharing
Conclusion
Medicaid Benefits FAQs
Medicaid benefits coverage provides healthcare assistance to eligible individuals and families who are unable to afford healthcare services.
The core Medicaid benefits include hospitalization, physician services, laboratory services, and home health services.
Optional Medicaid benefits can include services such as dental care, prescription drug coverage, and vision care, among others.
Eligibility for Medicaid benefits is typically based on income and other factors such as age, disability status, and family size.
Yes, it is possible to have private health insurance and still receive Medicaid benefits if you meet the eligibility requirements for both programs.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











