When it comes to navigating the world of Medicare, understanding the ins and outs of a Medicare appeal is of paramount importance for beneficiaries aiming to secure their rightful healthcare coverage. Essentially, a Medicare appeal is a structured process through which beneficiaries can challenge denied claims or decisions concerning their coverage made by the Medicare program. This process empowers beneficiaries by allowing them to contest decisions they believe are inaccurate or unjust, ensuring that they ultimately receive the coverage they are rightfully entitled to under their Medicare plan. The primary goal of a Medicare appeal is to rectify situations where beneficiaries feel that their claims have been unfairly turned down, and to ensure that the Medicare program lives up to its promise of providing appropriate and comprehensive coverage. Engaging in the appeals process can lead to both immediate financial relief and long-term benefits, making it an essential tool for safeguarding the healthcare rights and financial well-being of beneficiaries. Before diving into the appeals process, it's important to understand why claims might be denied. Denials can stem from a variety of reasons, including billing errors, medical necessity disputes, or incomplete documentation The process of appealing a denied claim is structured into multiple levels, each providing beneficiaries with an escalating platform to challenge these decisions. This layered approach ensures that different aspects of a claim's denial can be thoroughly addressed. At this level, beneficiaries or healthcare providers can request a review of the denied claim by the Medicare Administrative Contractor (MAC) that issued the initial decision. This step involves submitting additional information to support the appeal. If the claim is still denied after redetermination, beneficiaries can request a reconsideration by a Qualified Independent Contractor (QIC) who was not involved in the initial decision. Reconsideration involves an independent review of the claim. If the reconsideration decision remains unfavorable, beneficiaries can request a hearing before an Administrative Law Judge (ALJ). This formal hearing allows beneficiaries to present their case and provide evidence in support of their claim. Should the ALJ hearing not yield a satisfactory outcome, beneficiaries can request a review by the Medicare Appeals Council. This level involves a panel review of the ALJ's decision and the case record. If all other avenues are exhausted, beneficiaries can appeal the case in a federal district court. However, this level is typically pursued in cases involving significant financial implications or matters of broader legal importance. A notable advantage of launching a Medicare appeal lies in the opportunity to secure the coverage that beneficiaries rightfully deserve. Often, denials occur due to administrative glitches or misunderstandings. By appealing, beneficiaries can rectify these errors and ensure their rightful access to essential healthcare services. The financial aspect of Medicare appeals should not be underestimated. Denied claims can translate into unexpected out-of-pocket costs that can accumulate over time. A successful appeal not only relieves beneficiaries of these unwarranted financial burdens but also preserves their financial resources for other essential needs. Beyond financial implications, engaging in a Medicare appeal is a demonstration of asserting one's rights within the healthcare ecosystem. By challenging a denial, beneficiaries reinforce their entitlement to comprehensive coverage and emphasize their commitment to receiving equitable treatment under the Medicare program. One of the significant challenges of the Medicare appeals process is the time it takes to navigate through the various levels. Depending on the complexity of the case and the level of appeal, the process can be time-consuming and require patience from beneficiaries. Successful appeals often hinge on the availability of comprehensive and accurate documentation. Collecting the necessary medical records, billing documents, and other evidence can be challenging, especially for beneficiaries who are not familiar with the intricacies of medical documentation. While the appeals process offers a pathway to rectify denied claims, there is always a possibility that an appeal may not be successful. Factors such as the strength of the medical justification and the consistency of the evidence presented can influence the outcome of an appeal. When a claim is denied, it's essential to review the denial notice carefully. This notice provides critical information about why the claim was denied and outlines the steps required to initiate an appeal. Strong appeals often hinge on the availability of comprehensive medical records that support the medical necessity of the claimed service or treatment. Gathering these records and ensuring they are accurate and up-to-date is a crucial step in building a compelling case. The heart of a successful appeal is a strong medical justification. Beneficiaries should work closely with their healthcare providers to ensure that the appeal provides clear and convincing medical reasons for why the claimed service is necessary. Familiarity with Medicare policies and guidelines can give beneficiaries an edge in the appeals process. Understanding the criteria for coverage and the specific requirements for different levels of appeal can help beneficiaries navigate the process more effectively. When a claim is denied, beneficiaries may be left responsible for the entire cost of the denied service or treatment. These out-of-pocket costs can be unexpected and add up quickly, especially for more expensive medical services. Denied claims can have a significant long-term financial impact. Beneficiaries who forego necessary medical care due to denied claims might experience worsened health conditions over time, potentially leading to higher overall healthcare costs. Each level of the appeals process has specific timeframes within which beneficiaries must submit their appeal. It's crucial to adhere to these timeframes to ensure that the appeal is considered. Timely filing of appeals is essential to preserve the beneficiary's rights within the Medicare program. Failing to submit an appeal within the designated timeframe might result in the loss of the opportunity to challenge a denial. A successful appeal can lead to the approval of the previously denied claim. This outcome not only ensures that beneficiaries receive the necessary healthcare coverage but also relieves them of potential financial burdens. In cases where an appeal is denied, beneficiaries can explore alternative options. This might include seeking legal assistance or consulting with Medicare counseling services to explore further steps to address the denied claim. In the complex landscape of healthcare coverage, Medicare appeals stand as a vital tool for beneficiaries to advocate for their healthcare rights and financial well-being. From understanding the initial denial to navigating through multiple appeal levels, beneficiaries must equip themselves with knowledge and resources to effectively engage in the appeals process. Successfully appealing denied claims can lead to significant benefits, including securing deserved coverage, avoiding out-of-pocket expenses, and protecting one's rights within the healthcare system. However, it's important to recognize that the process may present challenges, such as complex documentation requirements and the possibility of unsuccessful appeals. Ultimately, engaging in the Medicare appeals process is a proactive approach that not only benefits individual beneficiaries but also contributes to upholding the integrity of the Medicare program as a whole.What Is a Medicare Appeal?
How Medicare Appeals Work
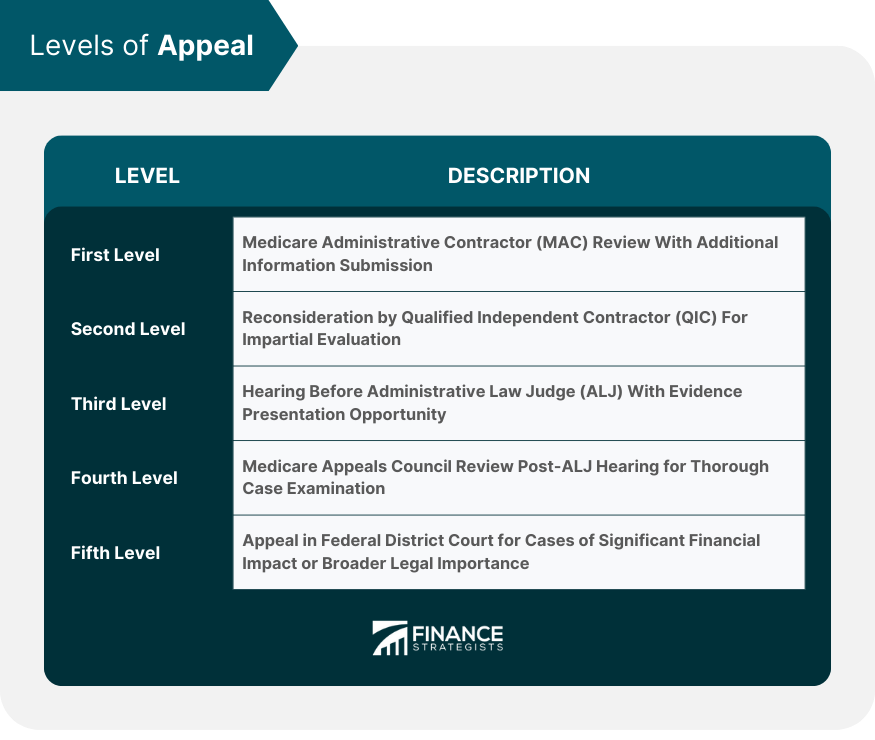
Levels of Appeal
First Level: Redetermination
Second Level: Reconsideration
Third Level: Administrative Law Judge Hearing
Fourth Level: Medicare Appeals Council Review
Fifth Level: Federal District Court
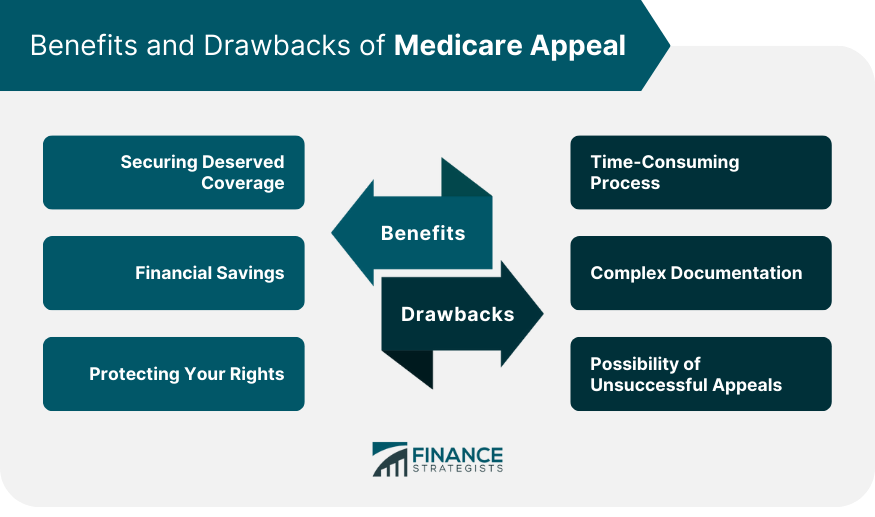
Benefits of Initiating a Medicare Appeal
Securing Deserved Coverage
Financial Savings
Protecting Your Rights as a Beneficiary
Drawbacks and Challenges of Medicare Appeals
Time-Consuming Process
Complex Documentation Requirements
Possibility of Unsuccessful Appeals
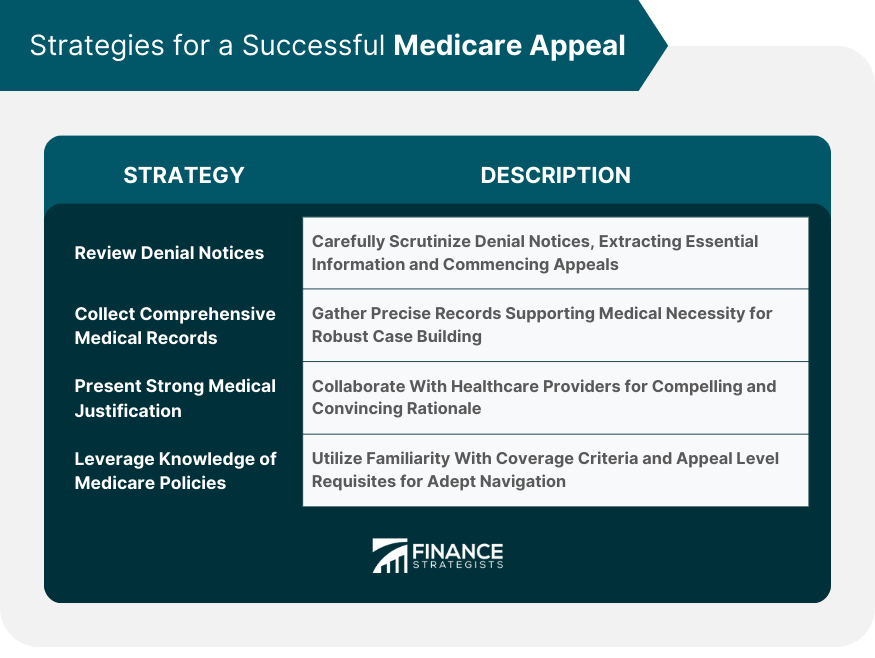
Strategies for a Successful Medicare Appeal
Reviewing Denial Notices Thoroughly
Collecting Comprehensive Medical Records
Presenting Strong Medical Justification
Leveraging Knowledge of Medicare Policies
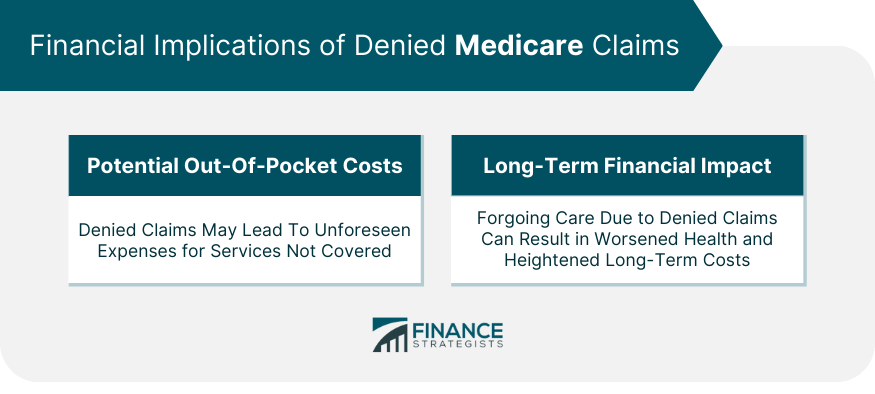
Financial Implications of Denied Medicare Claims
Potential Out-of-Pocket Costs
Long-Term Financial Impact
Timelines and Deadlines for Medicare Appeals
Appeal Timeframes for Each Level
Importance of Timely Filing
Appeal Decision Outcomes
Approval of Appeal and Positive Financial Impact
Dealing With Appeal Denials
Conclusion
Medicare Appeal FAQs
Medical appeals refer to the formal process through which individuals challenge denied medical claims or coverage decisions made by insurance providers.
Initiating a medical appeal allows you to contest decisions you believe are inaccurate or unjust, ensuring you receive the coverage you deserve for necessary medical services.
The process involves submitting an appeal to your insurance provider with additional evidence supporting your case. It often includes multiple levels, such as redetermination and reconsideration.
Successful medical appeals can lead to securing rightful coverage, relieving financial burdens, and protecting your rights as a patient within the healthcare system.
Medical appeals can be time-consuming, requiring patience. Gathering comprehensive documentation and facing the possibility of unsuccessful appeals are common challenges.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











