Medicare Part D is a voluntary prescription drug insurance program, designed to cover the costs of prescription medications for Medicare beneficiaries. Established by the Medicare Modernization Act of 2003, Part D aims to improve healthcare outcomes and reduce financial burdens associated with prescription drugs. Medicare Part D was introduced in January 2006, addressing the lack of comprehensive prescription drug coverage in the original Medicare program. Prior to Part D, many beneficiaries struggled with high out-of-pocket costs for medications, leading to poorer health outcomes and increased financial strain. The primary objective of Medicare Part D is to provide affordable and accessible prescription drug coverage for Medicare beneficiaries. The program aims to reduce financial barriers, promote medication adherence, and ultimately improve health outcomes for seniors and eligible disabled individuals. To be eligible for Medicare Part D, individuals must be enrolled in Medicare Part A and/or Part B, and reside in the plan's service area. There is no age limit for Part D enrollment, but most beneficiaries are 65 or older. Medicare Part D enrollment typically occurs during the Initial Enrollment Period (IEP), which starts three months before an individual's 65th birthday, includes their birth month, and ends three months after their birth month. Alternatively, beneficiaries can enroll during the Annual Enrollment Period (AEP), which runs from October 15 to December 7 each year. Special Enrollment Periods (SEPs) may be granted for specific situations, such as losing employer-based drug coverage, moving out of a plan's service area, or qualifying for Extra Help. SEPs allow individuals to enroll in a Part D plan outside of the standard enrollment periods. There are two types of Part D plans available: Prescription Drug Plans (PDPs): Stand-alone plans that supplement Original Medicare (Part A and Part B) by providing prescription drug coverage only. Medicare Advantage Plans with Prescription Drug Coverage (MA-PDs): These plans combine Medicare Part A, Part B, and Part D coverage into a single plan, typically offered by private insurance companies. When selecting a Part D plan, it is essential to compare coverage, costs, and benefits. Beneficiaries should consider: Formularies: Lists of covered medications, which may vary between plans. Network Pharmacies: Participating pharmacies where beneficiaries can fill their prescriptions. Costs: Premiums, deductibles, copayments, and coinsurance. Enrollment in a Part D plan can be completed online via the Medicare Plan Finder, by calling 1-800-MEDICARE, or by contacting the plan directly. Part D plans require monthly premiums, which may vary based on the chosen plan and income level. Some plans have an annual deductible, which must be paid before the plan begins covering prescription costs. Copayments are fixed amounts paid for each prescription, while coinsurance is a percentage of the medication's cost. These amounts can vary based on the plan and the drug tier. The coverage gap, commonly known as the "donut hole," occurs when a beneficiary's total drug costs exceed a certain threshold, leading to temporarily higher out-of-pocket costs. After reaching a second threshold, catastrophic coverage begins, and out-of-pocket costs decrease. Catastrophic coverage is activated when a beneficiary's out-of-pocket costs surpass a specific limit. At this point, the individual pays significantly lower copayments or coinsurance for the remainder of the year. Medicare Part D includes an out-of-pocket spending limit, which ensures that beneficiaries are protected from excessive drug costs. Once this limit is reached, the catastrophic coverage phase begins. The Low-Income Subsidy (LIS), also known as the Extra Help program, assists eligible individuals with limited income and resources in covering Medicare Part D costs, such as premiums, deductibles, and copayments. Some states offer State Pharmaceutical Assistance Programs (SPAPs) to help eligible residents pay for prescription drugs. These programs may provide additional financial assistance for Medicare Part D beneficiaries. Many pharmaceutical companies offer Patient Assistance Programs (PAPs) that provide free or low-cost medications to eligible individuals who cannot afford their prescriptions. Several non-profit and charitable organizations offer financial assistance, resources, and support to help Medicare beneficiaries with prescription drug costs. A coverage determination is a decision made by a Part D plan about the coverage or payment for a specific drug. Beneficiaries can request coverage determinations if they believe a drug should be covered, or if they disagree with the plan's cost-sharing requirements. Beneficiaries can request exceptions to a Part D plan's formulary, such as coverage for a non-formulary drug or a lower cost-sharing tier for a specific medication. If a coverage determination or exception request is denied, beneficiaries can initiate a multi-level appeals process to challenge the decision. A grievance is a complaint filed with a Medicare Part D plan. Grievances can address issues such as quality of care, customer service, or delays in processing requests. Individuals who are eligible for both Medicaid and Medicare are known as "dual eligibles." For these individuals, Medicare Part D serves as the primary payer for prescription drugs, while Medicaid may cover additional costs. If a beneficiary has employer or union health coverage that includes prescription drug benefits, coordination of benefits may occur between the employer or union plan and Medicare Part D. Medicare Part D may coordinate with other federal programs, such as TRICARE and Veterans Affairs (VA) benefits, to ensure beneficiaries receive comprehensive prescription drug coverage. Medigap policies, also known as Medicare Supplement policies, can help cover out-of-pocket costs for Medicare Part A and Part B but do not offer prescription drug coverage. Beneficiaries seeking prescription drug coverage must enroll in a separate Part D plan. Medicare Part D plans may change their formularies, costs, and coverage each year. Beneficiaries should review their plan options annually to ensure they have the most appropriate coverage. The Medicare Open Enrollment Period (OEP) runs from October 15 to December 7 each year. During this time, beneficiaries can review, compare, and switch their Medicare Part D plan or Medicare Advantage plan with prescription drug coverage. Special Enrollment Periods (SEPs) allow beneficiaries to make changes to their Medicare Part D coverage outside of the OEP in specific situations, such as moving out of a plan's service area or losing employer-based drug coverage. Changes in healthcare policy, legislation, and regulations can affect Medicare Part D's structure, benefits, and costs. Beneficiaries should stay informed about potential policy changes that may impact their prescription drug coverage. As the healthcare landscape evolves, Medicare Part D may face challenges such as rising drug prices, limited access to new medications, and increased demand for coverage. Potential improvements could include expanding access to lower-cost generic drugs, enhancing price transparency, and addressing the high cost of specialty medications. Maintaining and improving access to affordable prescription drugs is essential for Medicare beneficiaries' overall health and well-being. Medicare Part D plays a crucial role in ensuring that seniors and eligible disabled individuals can obtain the medications they need to manage their health conditions and maintain their quality of life.What Is Medicare Part D?
Eligibility for Medicare Part D
Criteria for Eligibility
Enrollment Periods and Deadlines
Special Circumstances for Eligibility
Medicare Part D Plans
Types of Part D Plans
Plan Comparison and Selection
How to Enroll in a Part D Plan
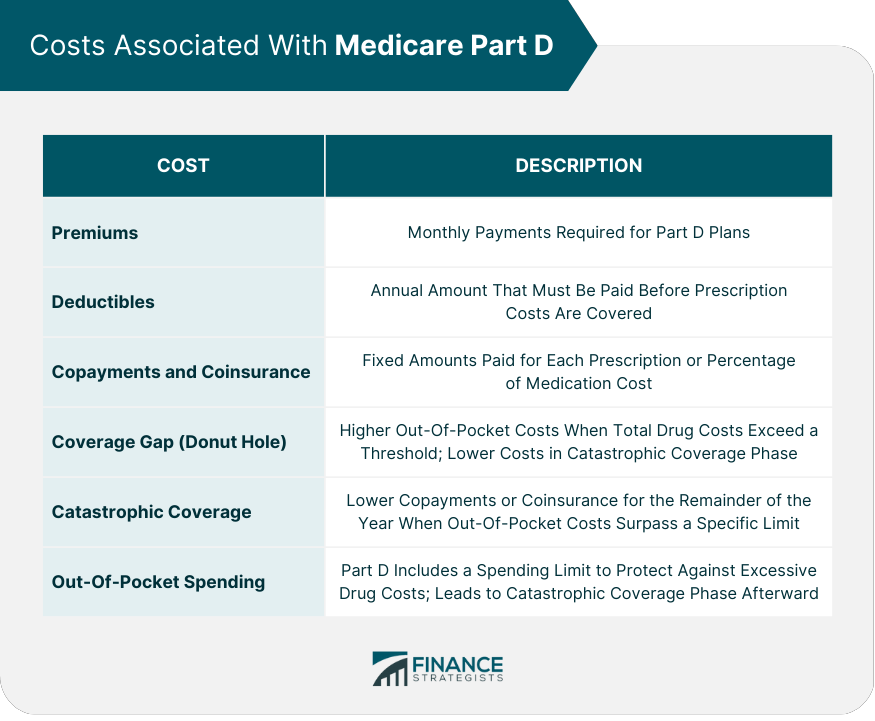
Costs Associated With Medicare Part D
Premiums
Deductibles
Copayments and Coinsurance
Coverage Gap (Donut Hole)
Catastrophic Coverage
Out-Of-Pocket Spending Limits
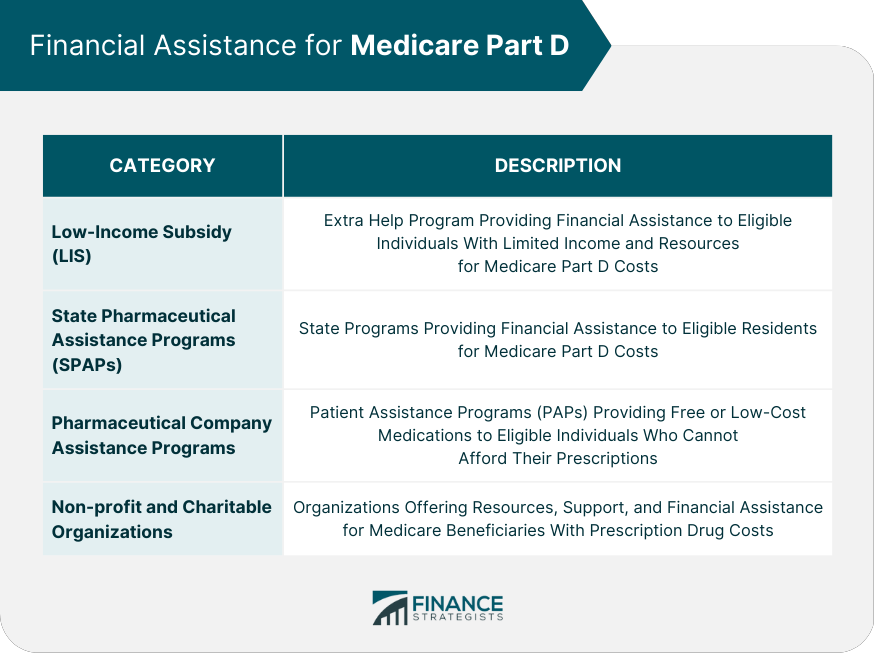
Financial Assistance for Medicare Part D
Low-Income Subsidy (LIS) / Extra Help Program
State Pharmaceutical Assistance Programs (SPAPs)
Pharmaceutical Company Assistance Programs
Non-profit and Charitable Organizations
Appeals and Grievances in Medicare Part D
Coverage Determination
Requesting Exceptions
The Appeals Process
Filing a Grievance
Coordination of Benefits
Medicaid and Medicare Part D
Employer or Union Health Coverage
TRICARE, Veterans Affairs, and Other Federal Programs
Medigap and Medicare Supplement Policies
Changes and Updates to Medicare Part D
Annual Plan Changes
Medicare Open Enrollment Period
Special Enrollment Periods
Final Thoughts
Impact of Healthcare Policy Changes
Challenges and Potential Improvements
Importance of Continued Access to Affordable Prescription Drugs
Medicare Part D FAQs
Medicare Part D is a federal program that provides prescription drug coverage to Medicare beneficiaries. The program is optional and is available to anyone who is eligible for Medicare.
Anyone who is eligible for Medicare, including those enrolled in Original Medicare (Parts A and B) or a Medicare Advantage plan, can enroll in Medicare Part D.
Medicare Part D is provided by private insurance companies approved by Medicare. Beneficiaries choose a plan that best fits their prescription drug needs, and the plan covers a portion of the cost of their prescription drugs.
Medicare Part D plans cover a wide range of prescription drugs, including those used to treat chronic conditions like diabetes, heart disease, and cancer. Each plan has its own formulary, or list of covered drugs, which can change from year to year.
The cost of Medicare Part D varies depending on the plan selected and the beneficiary's income. Beneficiaries typically pay a monthly premium for their Part D coverage, in addition to any deductibles, copayments, or coinsurance required by their plan. Low-income beneficiaries may be eligible for additional financial assistance to help cover the cost of their prescription drugs.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











