What Are Medicare Savings Programs (MSPs)?
MSPs are state-administered programs designed to help eligible low-income individuals and families with limited resources cover some of their Medicare costs, such as premiums, deductibles, and coinsurance.
The purpose of MSPs is to make healthcare more affordable and accessible for those who may have difficulty paying for their Medicare expenses.
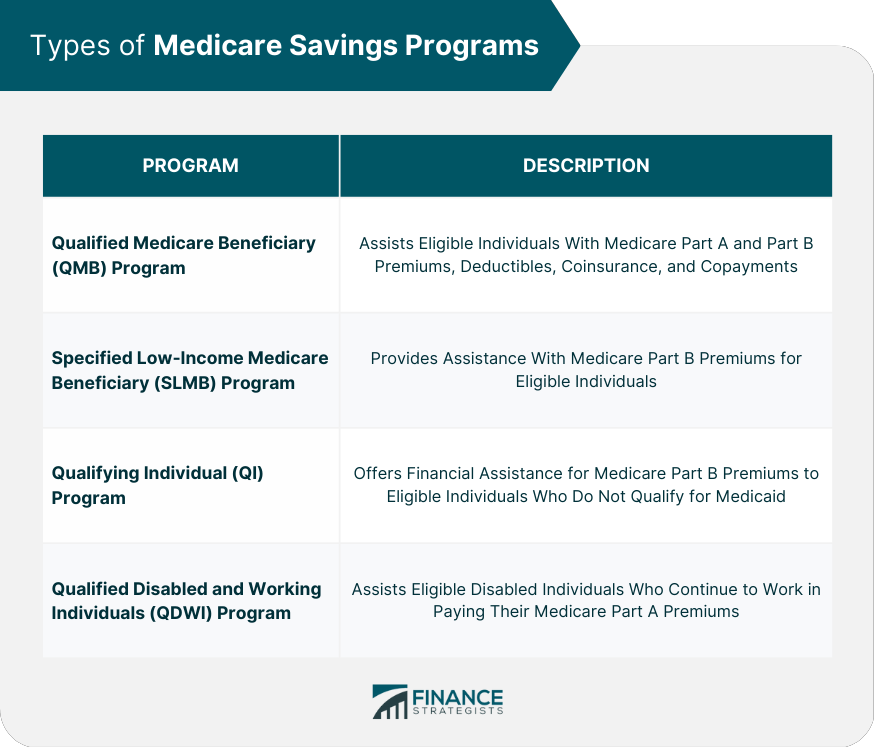
There are four main types of Medicare Savings Programs, each with distinct eligibility criteria and benefits:
Qualified Medicare Beneficiary (QMB) Program, Specified Low-Income Medicare Beneficiary (SLMB) Program, Qualifying Individual (QI) Program, and Qualified Disabled and Working Individuals (QDWI) Program.
Types of Medicare Savings Programs
Qualified Medicare Beneficiary (QMB) Program
The QMB program is the most comprehensive Medicare Savings Program. It pays for Medicare Part A and Part B premiums, deductibles, and coinsurance for individuals with incomes at or below 100% of the federal poverty level (FPL) and limited assets.
QMB beneficiaries are also protected from Medicare providers billing them for Medicare services that should be covered by Medicare.
Specified Low-Income Medicare Beneficiary (SLMB) Program
The SLMB program helps pay for Medicare Part B premiums for individuals with incomes between 100% and 120% of the FPL and limited assets. SLMB beneficiaries are not protected from providers billing them for Medicare services.
Qualifying Individual (QI) Program
The QI program also helps pay for Medicare Part B premiums for individuals with incomes between 120% and 135% of the FPL and limited assets. QI beneficiaries are not protected from providers billing them for Medicare services.
Qualified Disabled and Working Individuals (QDWI) Program
The QDWI program helps pay for Medicare Part A premiums for individuals with disabilities who have lost their premium-free Medicare Part A coverage because they returned to work. They must have a limited income and assets and meet other eligibility criteria.
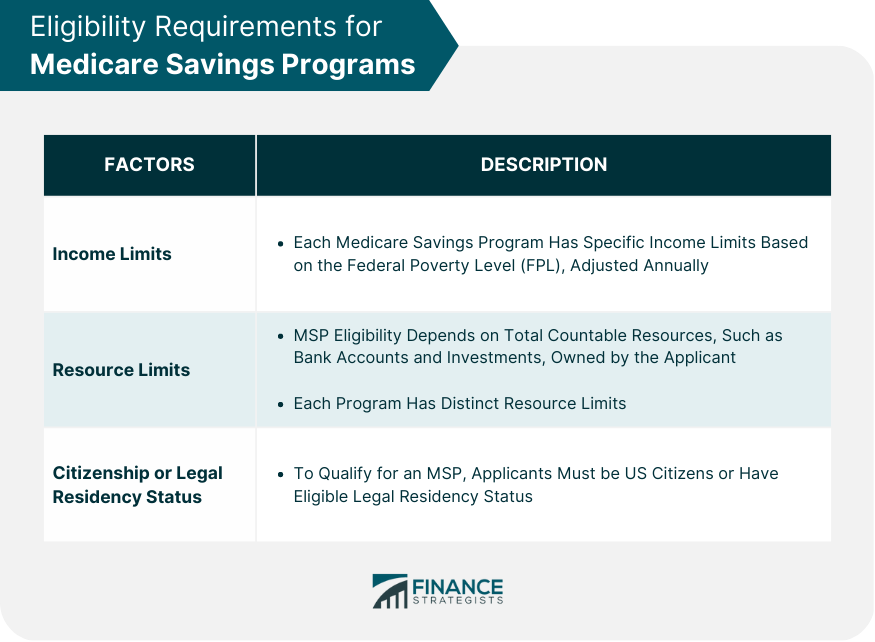
Eligibility Requirements for MSPs
Income Limits
Each Medicare Savings Program has specific income limits based on the Federal Poverty Level (FPL), which are adjusted annually.
Resource Limits
MSPs may also have resource limits, which are the total value of assets that an individual can have and still qualify for the program. Resource limits can vary depending on the program and the state.
Citizenship or Legal Residency Status
To be eligible for MSPs, individuals must be U.S. citizens or legal residents who have lived in the United States for at least five years. In some cases, individuals may also need to meet other eligibility requirements, such as being 65 or older or having a disability.
Benefits of Medicare Savings Programs
Premium Assistance
One of the primary benefits of MSPs is premium assistance. Depending on the program and the individual's income, MSPs can help pay for some or all of their Medicare Part A and/or Part B premiums.
This can be a significant cost savings for individuals who may struggle to afford their Medicare premiums on their own.
Deductibles, Coinsurance, and Copayments
MSPs can also help pay for other out-of-pocket costs associated with Medicare, such as deductibles, coinsurance, and copayments. This can be especially beneficial for individuals with chronic or complex medical conditions who may require frequent medical care.
Interaction With Medicaid Benefits
MSPs are administered by state Medicaid agencies, which means that individuals who qualify for MSPs may also be eligible for other Medicaid benefits.
For example, they may be eligible for Medicaid coverage of long-term care services, prescription drugs, or dental care. This can provide additional support for individuals who need assistance with their healthcare costs.
How to Apply for Medicare Savings Programs
Identifying Your State's Medicaid Agency
MSPs are administered by state Medicaid agencies, so the first step is to identify the agency in your state. This can be done by visiting the Medicaid website or calling the Medicaid hotline in your state.
Application Process
The application process for MSPs varies by state, but in general, individuals can apply by completing a paper application or by applying online. The application will require information about the individual's income, assets, and medical expenses.
Once the application is submitted, the state Medicaid agency will review it and determine if the individual meets the eligibility criteria for any MSPs.
Required Documentation
In addition to the application, individuals may need to provide certain documentation to verify their income, assets, and residency status. Required documentation may include tax returns, pay stubs, bank statements, proof of citizenship or legal residency, and proof of medical expenses.
Continuation and Termination of MSP Benefits
Annual Redetermination of Eligibility
MSP beneficiaries are required to undergo a redetermination of eligibility annually to ensure they still meet the program's income and resource requirements.
Reporting Changes in Income or Resources
Beneficiaries must report any significant changes in their income or resources to their state's Medicaid agency, as these changes may affect their MSP eligibility.
Termination of Benefits
MSP benefits may be terminated if a beneficiary no longer meets the eligibility criteria or fails to provide necessary documentation during the annual redetermination process.
Resources for Navigating Medicare Savings Programs
Government Resources
Government resources are available to help you understand and navigate Medicare Savings Programs:
Medicare.gov: The official government site for Medicare offers comprehensive information on MSPs, including eligibility, benefits, and application processes.
State Medicaid agencies: Each state's Medicaid agency administers MSPs and can provide guidance on eligibility, application procedures, and available benefits.
Non-profit Organizations
Non-profit organizations can offer support and assistance with MSPs:
State Health Insurance Assistance Programs (SHIPs): SHIPs provide free, unbiased counseling and assistance with Medicare-related issues, including MSPs.
Area Agencies on Aging (AAA): AAAs offer information and assistance with healthcare programs and services for older adults, including MSPs.
Professional Advisors
Professional advisors can help you navigate Medicare Savings Programs:
Social workers: Licensed social workers can provide guidance on healthcare options, including MSPs, and help with the application process.
Healthcare navigators: Healthcare navigators are trained professionals who assist individuals with understanding and accessing healthcare coverage options, such as MSPs.
Conclusion
Medicare Savings Programs play a critical role in making healthcare more affordable and accessible for individuals and families with limited income and resources.
Familiarizing yourself with the different MSPs, understanding their eligibility requirements, and successfully navigating the application process can help reduce your out-of-pocket costs and provide access to essential healthcare services.
It is crucial to stay informed about updates and changes to these programs, as well as to report any significant changes in income or resources that may affect your eligibility.
Utilizing available resources from the government, non-profit organizations, and professional advisors can provide invaluable support in navigating the complex MSP system.
By seeking guidance from these sources, you can better understand your healthcare options, maximize your benefits, and ensure you receive the healthcare coverage you need.
Ensuring access to affordable healthcare is a vital component of a healthy and secure future, and Medicare Savings Programs can serve as an essential lifeline for those in need of assistance.
Medicare Savings Programs (MSPs) FAQs
Medicare Savings Programs are financial assistance programs that help low-income Medicare beneficiaries pay for their Medicare premiums, deductibles, and other out-of-pocket costs.
To be eligible for Medicare Savings Programs, individuals must have Medicare Part A (hospital insurance) and meet certain income and asset requirements. The specific eligibility requirements vary by state, but typically individuals with incomes below a certain threshold and limited assets are eligible.
There are four types of Medicare Savings Programs: Qualified Medicare Beneficiary (QMB), Specified Low-Income Medicare Beneficiary (SLMB), Qualified Individual (QI), and Qualified Disabled and Working Individuals (QDWI). Each program has different eligibility requirements and provides different levels of financial assistance.
Medicare Savings Programs can help cover the costs of Medicare Part A and Part B premiums, deductibles, coinsurance, and copayments. Depending on the program, beneficiaries may also receive assistance with Medicare Part D (prescription drug coverage) premiums and cost-sharing.
To apply for Medicare Savings Programs, individuals should contact their state Medicaid agency or local Social Security office. Applicants will need to provide documentation of their income, assets, and Medicare enrollment. Once approved, beneficiaries will receive a notice of eligibility and any financial assistance provided by the program will be applied to their Medicare premiums and other costs.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.











